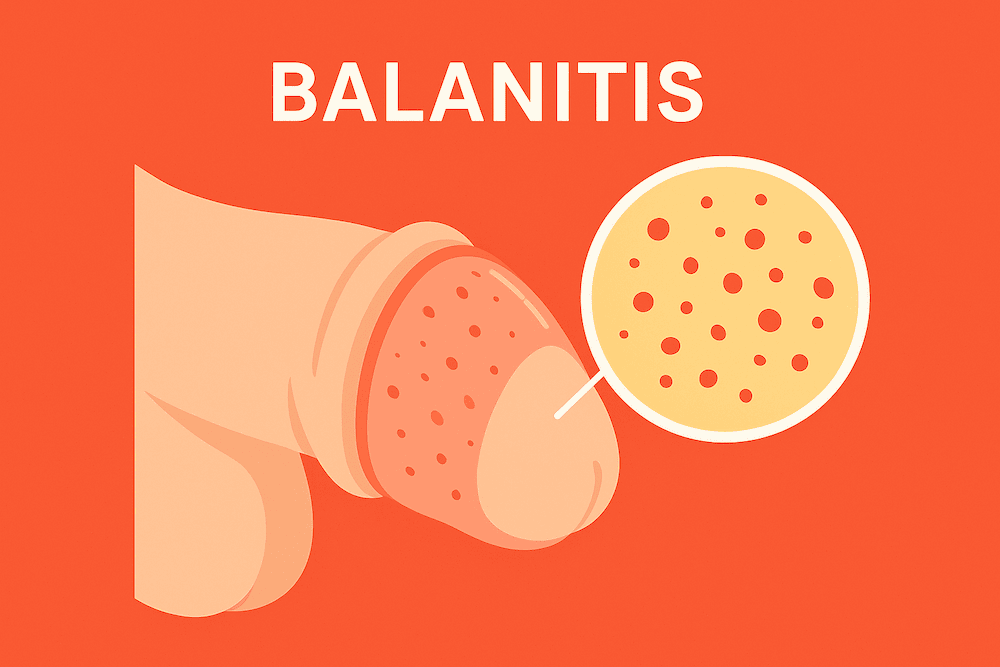
Balanitis might sound scary, but it’s actually a pretty common and treatable issue. Simply put, balanitis is inflammation of the glans (head) of the penis. It can happen to men of any age, whether you’re 18 or 80, circumcised or not , though it’s far more common if you haven’t been circumcised. In fact, an estimated 3% to 11% of males will experience balanitis at least once in their lives. So if you’re dealing with a red, sore, or itchy penis head, you’re definitely not alone. The good news is that balanitis is usually easy to manage with proper care and treatment.
Fun fact: The word “balanitis” comes from the Greek balanos, meaning “acorn,” referring to the glans’ shape. So yes , even ancient folks had to come up with a name for this condition!
Is Balanitis a STD?
One of the first questions guys often ask is whether balanitis is a sexually transmitted disease (STD). The short answer is no , balanitis itself isn’t an STD and you generally can’t catch balanitis from someone else through sex. The inflammation is usually due to irritation or an overgrowth of germs that are normally on your skin, rather than a specific “bug” that jumps from partner to partner. It also isn’t inherently contagious in and of itself.
However, (and this is a big however) certain sexually transmitted infections (STIs) can lead to balanitis or balanitis-like symptoms. For example, infections like gonorrhoea, chlamydia, syphilis, or herpes can cause inflammation of the penis that looks and feels like balanitis. In these cases, the STI is the underlying cause, and the balanitis is basically a symptom. So while you didn’t “catch” balanitis, you might have caught something else that triggered it. If you notice balanitis symptoms after unprotected sex with a new or high-risk partner, it’s wise to visit an std clinic and get checked. A doctor can run std testing to see if an STI (like the ones mentioned above, or others such as HPV or trichomonas) is present. This is important because you’ll want to treat the infection itself (with proper STD treatment) to fully resolve the balanitis and avoid passing anything to partners.
The bottom line: Balanitis isn’t classified as an STI, but it can be caused by infections, including STIs , so safe sex and regular check-ups (HIV testing and broader STI screens) are still key. And if your balanitis is due to an infection like yeast or bacteria, remember that those organisms can sometimes be passed on (for instance, yeast infections can transfer between partners). So don’t ignore symptoms , when in doubt, get it checked out.
What Causes Balanitis?
Balanitis can have a bunch of different causes. Often, it’s not just one thing , a combination of factors might be at play. Here are the most common causes and risk factors:
Poor Hygiene
Let’s be frank , not cleaning downstairs can lead to problems. If you don’t regularly clean under your foreskin (for uncircumcised men), sweat, urine, and dead skin cells can accumulate as smegma (a white, cheese-like buildup). This gunk is irritating and a breeding ground for germs. Poor genital hygiene is one of the leading causes of balanitis, as the constant irritation and bacterial overgrowth can spark inflammation.
Yeast Infections (Fungal)
The most frequent infectious cause of balanitis is a yeast infection , usually by Candida albicans, the same fungus that causes thrush. Yes, men can get yeast infections too! Candida normally lives in small amounts on our skin, but if it overgrows (often due to moisture and warmth under the foreskin), it can cause balanitis. This is sometimes called candida balanitis or “male thrush.” It’s not an STI; you can get it without sexual activity, though sexual transmission of yeast is possible. The telltale sign is a red, itchy rash often with a thick white discharge (kind of like cottage cheese) under the foreskin.
Bacterial Infections
Various bacteria can infect the glans/foreskin and lead to balanitis. Common culprits include those normally living on the skin that overmultiply in the wrong environment, or bacteria introduced from the gastrointestinal area (especially if hygiene is poor). Streptococcal and staphylococcal bacteria are frequently reported causes. These infections might cause more pus-like discharge and significant soreness. Again, most of these are not classic STDs , they’re often just everyday bacteria taking advantage of an opportunity.
Sexually Transmitted Infections
As mentioned, STIs deserve their own mention. Infections like gonorrhoea, chlamydia, syphilis, or genital herpes can present with balanitis or make you more prone to it. For instance, genital herpes can cause painful sores on the penis, and along with that you might get general inflammation (balanitis). If an STI is the cause, you’ll likely have other std symptoms too (such as urethral discharge or burning on urination in the case of gonorrhoea/chlamydia, or ulcers in the case of syphilis/herpes). Treating the infection will usually improve the balanitis as well.
Irritants and Allergens
Sometimes balanitis is caused by your skin freaking out due to irritation or an allergic reaction. The skin of the glans is sensitive, and a lot of things can set it off: harsh soaps or shower gels, scented lotions, deodorants or powders, detergents left in your underwear, and even the latex in condoms or chemicals in spermicidal jellies. If you have sensitive skin, something as simple as a new soap or not rinsing well after washing can cause redness and itching. Overly vigorous washing or scrubbing can also inflame the area , moderation is key when cleaning (more on hygiene later).
Skin Conditions
Sometimes, an underlying dermatological condition is the culprit. Conditions like eczema, psoriasis, lichen planus, or lichen sclerosus (also known as balanitis xerotica obliterans when on the penis) can affect genital skin and cause balanitis-like inflammation. These often cause chronic irritation or distinctive changes in the skin (for example, lichen sclerosus can cause white patchy areas). These aren’t infections, but they still require medical treatment (often with prescription creams) to manage.
Medical Conditions
Certain health issues can increase your risk of balanitis. A big one is diabetes , especially if it’s not well-controlled. High blood sugar can lead to sugar being present in urine, and when that urine drops get trapped under the foreskin, it’s like candy for yeast and bacteria. Diabetic men (particularly if uncircumcised) often experience recurrent balanitis unless they keep both their blood sugar and hygiene in check. Another condition linked to balanitis is reactive arthritis (formerly Reiter’s syndrome), which is an autoimmune condition that can cause balanitis as one of its symptoms. Additionally, obesity can be a risk factor (harder to maintain hygiene, more skin folds and moisture).
Phimosis
This is both a risk factor and sometimes a result of balanitis. Phimosis means a tight foreskin that can’t be easily retracted (pulled back) over the glans. Men with a naturally tight foreskin or scarred foreskin often struggle to clean underneath, leading to the buildup of irritants and germs. That in turn causes balanitis. It’s a vicious cycle: phimosis can cause balanitis, and frequent balanitis can cause scarring that worsens phimosis. If you have this issue, pay extra attention to gentle hygiene. In severe cases, a doctor might recommend treatments to loosen the foreskin or circumcision (more on that later).
In many cases, it’s a mix: for example, a guy with poor hygiene and mild phimosis might develop a Candida infection , that’s three factors all contributing at once. This is why it’s best to see a healthcare professional for diagnosis if you’re not sure what’s causing your symptoms. They can identify the root cause (or causes) and guide you on proper treatment.
Symptoms of Balanitis
So, how do you know if you have balanitis? The symptoms are usually pretty hard to ignore. They can vary from mild to downright painful, depending on the cause and severity. Common symptoms of balanitis include:
- Redness or Rash: The glans (and sometimes the inner foreskin) often looks red, inflamed, or irritated. It might be a uniform redness or patchy. The area can also appear shiny or have red spots/rash.
- Soreness or Pain: The tip of your penis might feel tender to touch, sore, or even painful, especially during activities like sex or when urine touches the inflamed skin. Some men describe a burning sensation.
- Itching or Burning: Persistent itchiness is a frequent complaint. You might have the urge to scratch (try not to, as that can worsen things). A general burning feeling in the glans is also common.
- Swelling: The head of the penis and/or foreskin can become swollen or puffy, making the penis look bloated. Swelling is basically your body’s way of reacting to the inflammation.
- Discharge: You may notice discharge coming from under the foreskin. It can be thick and white (often a clue for yeast infection) or yellow/greenish (possibly bacterial). The discharge can cause clumping or a gooey film on the glans. Often this goes hand-in-hand with a bad smell.
- Unpleasant Odor: Because of the buildup of smegma and germs, balanitis can cause a foul smell. If you notice a strong, fishy or yeasty odor from your groin, it could be a sign of infection under the foreskin.
- Foreskin Problems: You might have trouble retracting your foreskin (phimosis) if it’s become too tight or swollen. Sometimes, even if you previously had no issues, the inflammation can make it harder to pull back. In severe cases, if you do retract, the foreskin might get stuck behind the glans (this is paraphimosis , an emergency , but it’s pretty rare just from balanitis alone). Generally, any difficulty with the foreskin moving normally is a red flag.
- Painful Urination: If the opening of the urethra (where urine comes out) is inflamed, you could feel a sting or burn when you pee. Also, if swollen foreskin blocks the flow a bit, the pressure can cause pain when urinating. Some men find they have to adjust how they pee because it’s uncomfortable.
- Sores or Blisters: In some cases, you might see small sores, ulcers, or blisters on the glans or foreskin. This is more common if an infection like herpes is involved, or if balanitis is severe and the skin has started to crack or ulcerate. These can be quite painful and may bleed or ooze.
- General Ill Feeling (Rare): Balanitis itself usually stays local to the penis. However, if it’s due to a bad infection, you might feel unwell , for example, with an fever or swollen groin lymph nodes in very severe cases. This isn’t typical for simple balanitis, but it’s possible if an infection is raging.
Remember, balanitis symptoms can resemble symptoms of some STIs and other conditions. For instance, genital herpes can cause pain, redness, and sores; syphilis can cause sores; some skin conditions can cause redness and itching. That’s why getting a correct diagnosis is important. Don’t just self-diagnose based on Dr. Google , if you have persistent symptoms, see a doctor. They might take a look, ask about your hygiene habits, and possibly take a swab or urine test to check for infections. Balanitis is usually diagnosed by physical exam (doctors know it when they see it), but tests can help pinpoint the exact cause.
On the bright side, most cases of balanitis clear up pretty quickly once you start the right treatment. Which brings us to…
How Is Balanitis Treated?
Treating balanitis is typically straightforward , the main goals are to resolve the inflammation and address whatever caused it in the first place. The exact treatment can vary depending on the cause (infection vs. irritant vs. underlying condition), but here are the usual steps and remedies:
Improved Hygiene (Gentle Cleaning)
No matter what caused your balanitis, the first step is usually to clean the area properly. Start washing the glans and foreskin daily with lukewarm water. Gently pull back the foreskin (if it retracts) and clean underneath. Avoid harsh soaps or perfumed shower gels on the penis for now , they can irritate raw skin. Instead, you can use a mild, unscented soap or an emollient (moisturizing cleanser) if needed, or just warm water. After washing, dry the area gently and thoroughly (pat dry with a clean towel or let it air dry for a moment) because moisture can promote yeast and bacteria growth. During treatment, also avoid activities that could further irritate the area , for example, you might want to hold off on sex or masturbation until things calm down.
Topical Medications
Based on the cause, your doctor may prescribe creams or ointments to apply to the affected area:
- Antifungal Creams: If your balanitis is due to a yeast (Candida) infection, antifungal creams are the go-to. Common ones include clotrimazole (you might know it as Canesten cream) or miconazole. These are applied to the glans and foreskin a couple of times a day for one to two weeks. For more stubborn yeast infections, an oral antifungal like fluconazole might be prescribed. Many antifungal creams are available over-the-counter, but it’s best to see a doctor first to be sure you indeed have a yeast infection. With treatment, a fungal balanitis often clears up in about a week or so.
- Antibiotic Creams or Pills:If a bacterial infection is causing your balanitis, you’ll need antibiotics. For mild cases, a cream like mupirocin might be enough. If it’s more severe, or you have systemic symptoms, oral antibiotics (such as amoxicillin or others appropriate to the infection) may be given. The specific antibiotic will depend on what bacteria is suspected , sometimes the doctor might take a swab to identify the bacteria. It’s important to use the antibiotic for the full course, even if things start to look better in a few days, to make sure the infection is fully gone.
- Steroid Creams: These are anti-inflammatory creams (typically mild corticosteroids) that help reduce redness, swelling, and itching. If your balanitis is caused by irritants, allergies, or a skin condition (like eczema/psoriasis), a steroid cream such as 1% hydrocortisone might be recommended. In some cases, doctors prescribe a combination cream that has both an antifungal and a steroid, since reducing inflammation can ease symptoms while the underlying infection is being treated. Important: if an infection (like candida or bacteria) is present, steroids are usually used alongside an anti-infective, not alone, because steroids alone could dampen your immune response and actually worsen an untreated infection. So don’t just slather on leftover steroid cream you might have at home, get medical advice on this.
Treating Underlying Causes
If your doctor finds out an underlying cause, that will be addressed too:
- If an STD is the culprit, you’ll get appropriate medication for that infection (e.g., antibiotics for gonorrhoea or syphilis, antivirals for herpes). Clearing the STI will in turn resolve the balanitis. Make sure your sexual partner(s) get treated too, if applicable, to avoid ping-ponging an infection back and forth.
- If diabetes is a factor (and you have high blood sugar), you may need to work with your doctor on better diabetes control. This could involve adjusting medications or diet to bring your blood glucose to target levels. Better sugar control will help prevent future episodes of balanitis.
- If an irritant or allergen caused it, obviously stop using whatever product seemed to trigger your balanitis. Your doctor might help identify what it was if it’s not obvious. Sometimes it’s trial and error , e.g., switch to hypoallergenic soaps, or latex-free condoms if you suspect a latex allergy, etc.
- For skin conditions like lichen sclerosus or psoriasis, you might be referred to a dermatologist or given specialized creams (stronger steroids, immune-modulating creams, etc.) to manage the condition long-term so that balanitis doesn’t keep recurring.
Pain Relief
Balanitis can be uncomfortable, so managing symptoms is part of treatment. Soaking the penis in lukewarm salt water can be soothing (salt baths). Over-the-counter pain relievers like acetaminophen or ibuprofen can help if it’s particularly sore. Just be gentle with the area; wearing loose, breathable underwear and pants can also make a big difference in comfort during recovery.
Circumcision (Rare Cases)
For most men, balanitis will resolve with the above measures. But in recurrent or very stubborn cases, especially if you have chronic phimosis, a circumcision might be recommended as a more permanent solution. Circumcision is a minor surgical procedure to remove the foreskin. Without a foreskin, the environment that allowed balanitis to keep happening (trapped moisture, difficult hygiene) is eliminated. This is usually a last resort if you keep getting balanitis repeatedly and other treatments haven’t helped, or if your foreskin has become fibrosed (scarred) and non-retractable from long-term issues. It’s definitely something to discuss with a urologist rather than jump into lightly. Some men find that once they’ve been circumcised, the balanitis issue goes away for good. Others prefer to manage it with hygiene and medications if possible. There’s also a less drastic procedure called a dorsal slit (a small cut to loosen the foreskin) that can be considered in certain cases, but this is uncommon.
In most situations, balanitis should start improving within a few days of treatment and clear up within ~1 to 2 weeks. Just remember to complete the full course of any medication even if you feel better sooner. And absolutely avoid sexual contact until you’re healed (both for your own comfort and so you don’t expose a partner to any infection you might have).
If you’ve completed treatment and the balanitis still isn’t going away, go back to the doctor. They might need to do further tests or consider other causes (like a biopsy to rule out an unusual condition, which is rare). But again, that’s seldom needed , the vast majority of cases get resolved with the basic treatments above.
Preventing Balanitis
Once you’ve had balanitis, you probably won’t want it again , and even if you haven’t, it’s worth taking steps to prevent it. Prevention is largely about good hygiene and avoiding things that irritate your penis. Here are some practical tips for keeping balanitis at bay:
Clean Yourself Properly
Wash your penis daily with warm water. If you’re uncircumcised, gently pull back your foreskin and rinse underneath. You don’t need harsh soap , in fact, plain water or a mild unscented soap is best. (If you do use a bit of soap, rinse thoroughly so none is left behind.) After washing, dry the area well. A moist environment under the foreskin is prime real estate for bacteria and yeast to grow, so you want things clean and dry. Tip: after a shower, pat the penis dry with a towel and maybe even wait a minute before putting on underwear to ensure no dampness remains.
Avoid Irritants
Steer clear of perfumed soaps, lotions, or powders on your genitals. These often cause irritation. Use gentle, hypoallergenic products for the groin if possible. Also, if you’ve had issues with certain condoms or lubes, consider alternatives. For example, if you suspect a latex allergy or irritation, try latex-free condoms (there are polyurethane and polyisoprene options). If a certain lubricant gave you a burning feeling, switch to a simpler, water-based, glycerin-free formula. Everyone’s skin is different , the key is to notice if something consistently causes you redness or itch, and discontinue using it.
Practice Safe Sex
While balanitis isn’t an STI, unsafe sex can expose you to infections that cause balanitis. Using condoms every time with new or casual partners will help protect you from STIs like gonorrhoea, chlamydia, syphilis, herpes, and HIV. Fewer infections = lower chance of getting balanitis as a side effect. Safe sex is just a good practice overall for your sexual health. Also, get std testing regularly if you’re sexually active with multiple partners, so any asymptomatic infections can be caught and treated early. (Untreated STIs can sometimes simmer quietly and then show up as balanitis or other complications down the line.) Bottom line: use protection and stay on top of your sexual health , it’s a win-win for you and your partners.
Manage Underlying Conditions
If you have diabetes, keeping your blood sugar well-controlled will help hugely. As mentioned, high sugar in urine feeds yeast and bacteria, so aim for good glucose control to prevent those balanitis-causing infections. If you’re overweight, weight loss can help reduce sweating and improve hygiene. Any other chronic skin conditions or allergies , follow your doctor’s advice in managing those, especially if they tend to affect your groin area.
Careful After Urination and Sex
After you urinate, if you’re uncircumcised, consider dabbing the tip of the penis with toilet paper to dry off any drops (rather than just shaking and pulling up underwear). This prevents moisture accumulation. After sex or masturbation, it’s a good idea to wash your penis (or at least rinse) to remove any bodily fluids or lubricant that could be irritating if left on the skin. This isn’t about being squeaky clean 24/7, just basic care.
Do Not Force the Foreskin (For Parents and Men)
If you have a young son, never forcibly retract his foreskin , in young boys, the foreskin may not retract fully and that’s normal. Forcing it can cause small tears and lead to balanitis. Teach gentle hygiene as he gets older. For adult men: if your foreskin is tight, be gentle. If you can’t retract it easily, talk to a doctor for advice; don’t force it and injure yourself. Gradual stretching exercises or medical treatments can sometimes loosen a tight foreskin over time.
By following these prevention tips, you’ll greatly reduce your chances of getting balanitis. Essentially, keep things clean and dry, avoid harsh chemicals, have safe sex, and manage any health issues that could contribute. These habits are beneficial not just for preventing balanitis, but for good genital health in general.
What If You Don’t Treat It? (Complications of Balanitis)
Balanitis is usually easy to treat, but what happens if you ignore it or it keeps coming back frequently? Let’s say someone just lives with the discomfort or tries to self-treat without addressing the real cause , there are a few potential complications and long-term issues that could arise:
Chronic Pain and Discomfort
First off, untreated balanitis can turn into a chronic issue , meaning that redness, irritation, and pain might persist or flare up repeatedly. This can obviously put a damper on your day-to-day life and sexual activity. Some men with chronic balanitis find sex painful or start avoiding intimacy because of the discomfort, which can even lead to temporary sexual dysfunction or trouble maintaining erections due to the pain and anxiety it causes. In other words, ignoring balanitis can potentially hurt your sex life.
Phimosis (Tight Foreskin)
Ongoing inflammation can cause scar tissue to form. Over time, this scarring can lead to phimosis, where the foreskin becomes so tight that you cannot retract it at all. Even if you never had phimosis before, repeated bouts of balanitis can scar the foreskin and reduce its elasticity. Phimosis not only makes hygiene even harder (potentially causing a vicious cycle of more infections), but it can also interfere with sex or even normal urination in severe cases. Once scar tissue forms, conservative treatments might not work and circumcision could end up being the only fix.
Paraphimosis
This is a less common but serious issue. Paraphimosis happens typically if you do retract a tight or swollen foreskin and then it gets stuck behind the glans and cannot go forward again. The foreskin acts like a tight rubber band strangling the head of the penis. Severe balanitis swelling could contribute to this if one isn’t careful. Paraphimosis is an emergency , it can cut off blood flow. You’d notice the glans becoming very swollen, painful, and bluish. It requires prompt medical attention to reduce the foreskin back. Chronic balanitis increases the risk of this because of the combination of swelling and tightness.
Balanitis Xerotica Obliterans (BXO)
Despite the intimidating name, this is essentially the penile manifestation of lichen sclerosus , a chronic inflammatory skin condition. Long-standing balanitis (especially if related to lichen sclerosus, which some experts think can be triggered by chronic irritation) can lead to white, shiny patches on the glans or foreskin that characterize BXO. BXO can cause the skin to become inelastic and fibrous. It often leads to phimosis and can even extend to cause meatal stenosis (narrowing of the urethral opening). If the urine opening scars and narrows, you might experience a weak urine stream or spraying and need a procedure to fix it. BXO is usually diagnosed via biopsy and has its own treatment protocols, but the key point is that untreated inflammation might contribute to its development.
Urethral Strictures and Urinary Issues
Apart from meatal stenosis, severe ongoing inflammation can, in rare cases, cause scarring further down in the urethra (the tube that carries urine out). This is called a urethral stricture. It’s not common from balanitis alone, but if infection spreads or inflammation is severe, it’s possible. Strictures cause difficulty urinating and may require surgical procedures to correct.
Increased Risk of Penile Cancer
This is the complication that sounds the scariest, but keep in mind it’s very rare. Chronic inflammation anywhere in the body can sometimes increase cancer risk, and the penis is no exception. Men with a history of long-term untreated balanitis, phimosis, or BXO have a slightly higher risk of developing penile cancer later on. Some statistics have shown that a notable percentage of penile cancer patients had a history of chronic balanitis or phimosis. The thought is that constant inflammation and cell turnover might predispose cells to become cancerous over many years. Important: Penile cancer itself is quite rare, and having had balanitis does not mean you’re going to get cancer. It’s just one of those “increased risk” factors. By treating balanitis promptly and not letting it become chronic, you essentially eliminate this concern. If you ever notice unusual growths, persistent sores, or changes in the color/thickness of skin on your penis, get it checked , but again, cancer is an unlikely outcome, especially if you take care of your health.
As you can see, most of these complications come from neglecting the problem. Balanitis, in its acute form, is usually easy to fix. It’s when people don’t address it, or it keeps coming back frequently without proper prevention, that these longer-term issues can appear. The best way to avoid complications is to treat balanitis early and follow those prevention tips to stop it from becoming a recurrent issue. If you have a condition like phimosis or BXO that predisposes you to balanitis, working with a doctor (possibly a urologist or dermatologist) to manage that will be crucial.
When to See a Doctor
You should consider seeing a healthcare provider as soon as you notice persistent balanitis symptoms (give it a day or two of gentle home care , if it’s not clearly improving, get medical advice). Definitely see a doctor if:
- It’s very painful, or you have trouble urinating.
- You see blisters, open sores, or significant discharge (could be an STI or severe infection).
- You develop fever, chills, or feel ill, which could indicate the infection is more serious.
- The symptoms keep coming back despite you trying to prevent them.
- You have never been able to retract your foreskin or it has gradually become tighter (you might need evaluation for phimosis).
- Over-the-counter antifungals or hygiene measures aren’t working at all after a few days.
Medical professionals are used to seeing these issues, so don’t be embarrassed. Balanitis is a common men’s health problem, and doctors (whether a GP, dermatologist, or urologist) can quickly help you get relief. They may also test for diabetes or STIs if appropriate, to address any underlying causes.
Take Control of Your Sexual Health
Balanitis might be uncomfortable and inconvenient, but it’s not the end of the world. It’s a common condition involving inflammation of the penis head, often affecting men who are uncircumcised, have poor hygiene habits, or underlying infections. The key takeaways are: keep things clean, avoid harsh irritants, practice safe sex, and treat any infections or medical issues that could be fueling the inflammation. Most cases resolve with simple measures like topical creams and good hygiene, and it usually clears up within a couple of weeks with treatment.
Ignoring balanitis is the worst thing you can do , not only will you be miserable longer, but you risk complications like foreskin problems or other infections. On the flip side, addressing it promptly will have you back to normal in no time and help you prevent future bouts.
If you’re in Singapore (or anywhere, really) and dealing with balanitis symptoms, don’t hesitate to reach out to a doctor. Clinics like Shim Clinic in Singapore are experienced in men’s sexual health issues and can provide confidential, professional care. Whether it’s a quick check-up for a yeast infection or a full screening for STIs, getting the right diagnosis and treatment will put your mind at ease and get rid of the problem. Remember, your penis is telling you something when it’s red or sore , listen to it! Take care of your manhood with the same attention you’d give to any other important part of your body.
In short, balanitis is beatable. With the right care and a few lifestyle tweaks, you can keep your penis healthy, infection-free, and ready for action. If you suspect you have balanitis, take action now , your future self (and your partners) will thank you. Stay clean, stay safe, and don’t be afraid to seek medical advice when you need it. Your health is worth it.
If you are experiencing symptoms of balanitis or any other sexual health concern, Shim Clinic in Singapore offers discreet care. Our doctors provide comprehensive STD testing, STD treatment, and support for conditions such as erectile dysfunction, premature ejaculation, and HIV prevention. Reach out today and protect your health with confidence.